A $1.2 million federal grant was given to the MU Department of Health Psychology to help expand the department’s program that trains interns to fight against the opioid epidemic in rural Missouri.
“This will enable us to train interns to intervene early before opioid use disorder occurs among high risk populations,” Laura Schopp, department chair and professor of health and psychology, said.
The Graduate Psychology Education program gives hands-on internships to doctoral psychology students and allows them to work in rural areas where access to mental healthcare is difficult. The grant will allow an additional 21 predoctoral interns to join the program over the next two years.
“We are finding ourselves needing to work hard to catch up with the demand for services in this area,” Schopp said.
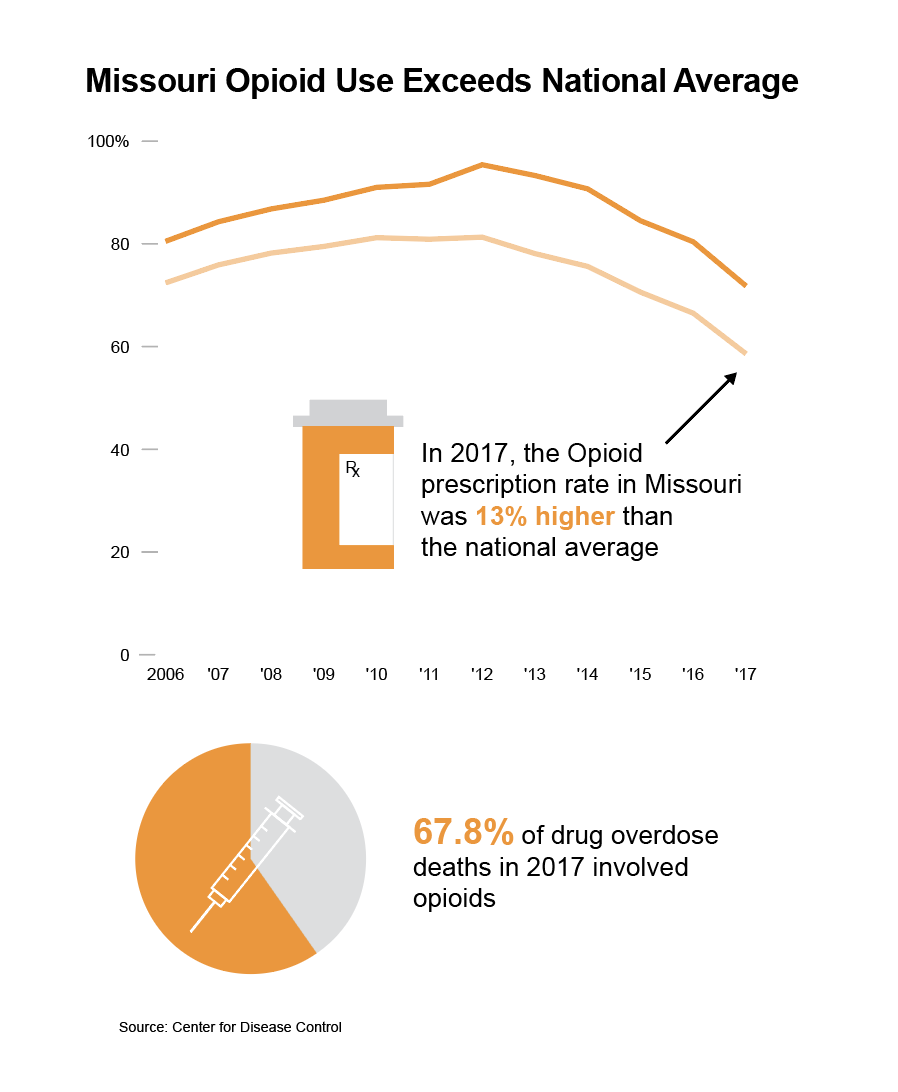
According to the National Institute on Drug Abuse, the rate of opioid-involved overdose deaths in 2017 was higher in Missouri than the national rate. Schopp said this might be due to Missouri having a high rural poverty rate, a higher prevalence of serious mental health issues and difficulties in growing its prescription drug monitoring program.
However, it’s the lack of access rural Missourians have to healthcare that’s making the opioid epidemic so impactful.
“The cities are pretty well covered in terms of health care, but the rest of the state is kind of on its own, and that presents challenges for patients and providers,” John Lace, Saint Louis University doctoral student, said.
To earn his Ph.D. in clinical psychology, Lace has to complete a year-long internship working in the field. Lace was matched up with MU’s program and is now working with Schopp and the Department of Health Psychology.
“I’ve seen patients from as far away as four and a half hours down from the bootheel that come up here for services since they’re so far away,” Lace said.
Even though rural areas face distance barriers, urban areas face problems as well.
“There are not enough treatment providers, especially treatment providers who can treat high-need, low-income patients,” Schopp said.
This program is trying to solve that.
“Twenty one interns alone, 21 newly minted psychologists will not address this issue for Missouri, but it will certainly provide a cadre of trained psychologists who can lead in ensuring that we provide the right access in the future,” Schopp said.
Schopp said 80% of the interns that have gone through the program have gone on to work in these underserved regions.
“The biggest thing I’ve learned is how to integrate rural healthcare and mental healthcare into my practice,” Lace said.
Lace and other interns in the program go through “intensive” training, as Schopp puts it. They learn brain behavior relationships and management of chronic health conditions from a behavioral health perspective. The program has interns looking closely at neurological disorders since people with those disorders are often at risk for chronic pain symptoms and therefore substance abuse.
“I find a lot of personal value in being able to connect with people who need help with one thing or the other, being able to be really present with them in that moment and acknowledge them in their difficulties and then actually help them out,” Lace said.
_Edited by Laura Evans | [email protected]_